The Future of Radiation Oncology: A Numbers Game We Can’t Ignore
"Its tough to make predictions, especially about the future" - Yogi Berra
A few forum discussions (Would you apply today? and Rad onc is the only specialty in medicine I could see myself doing, what should I do?) and a Red Journal article, Changes in employment and practice locations among radiation oncologists: 2015 – 2023, got me thinking. Let’s dive into the interesting part of the article (this post will not be an in-depth review).
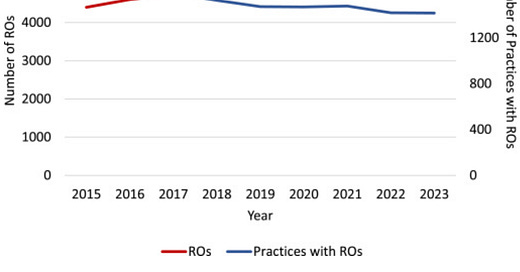
The number of practicing ROs increased by 16%, from 4,399 to 5,087, and the number of practices that employed ROs decreased by 13%, from 1,620 to 1,416, between 2015 and 2023
So, this tracks—there are many more of us, 16% more than a decade ago. More join the workforce than retire. And we are working for larger groups / hospital systems - i.e. evidence of consolidation.
I’ve been sounding the alarm about supply issues for a long time and have compared it to climate change—where we see changing weather patterns that tell us not to worry (“All my residents got jobs and they are starting at $500k!”), but there are telltale signs that something is off. What makes me think something is off? First of all, to earn the same amount of money, we see many more patients. many more patients. This is a systemic issue that aligns with changes in fractionation and the reimbursement adjustments of 2015. But, something else I am seeing is even more concerning. I know plenty of people that do not get to a number of RVUs that would correlate with their income. Another way of saying this - say your threshold is 9,000 RVUs per year and you make a base salary of $540,000 a year with a $60/RVU bonus after 9,000 RVUs. There are many physicians below their threshold and there is no downward adjustment to their base salary. Why? Well, the specialty remains lucrative to the hospital.
With modern treatment, the professional fees are about 17% and the technical fees are about 83%. I.e. if you are earning $500,000 in professional fees, the hospital is earning about $2.5 million in technical fees. Even with labor and capital costs, this is a huge chunk of change and any well managed department is very profitable compared to other departments in the hospital. Radonc has routinely subsidized less lucrative parts of the hospital ecosystem. If they adjust the salary downward or put the doctor on a pure production model, they risk losing the physician. So, they subsidize their salary with a part of the technical revenue. Doing this contractually is not allowed, but if done as a negotiated base salary, it’s kosher. I see this at many centers - including ones I’ve worked for in the past and where I work now. If you have a competent and compassionate radonc that plays well in the hospital sandbox (as most of us tend to be) and they aren’t super busy, there is rarely pressure to increase their volumes or directives to reduce their base. Hospitals are smart to do this, because we generate downstream revenue and it allows them to have a comprehensive cancer center where surgery, chemotherapy and radiation can all be administered in-house. The technical revenue makes it worth it. But can this last?
Here is what we know:
Radiation oncologist supply has increased (16% in above study)
Cancer incidence has risen slightly. Based on data I have, from 2015 to 2021, cases have gone from 440 cases per 100,000 to 458 cases per 100,000 - about a 4% rise. Check my work if you’d like.
Our indications are going down and our consult/treatment numbers are going down, per patient. I have written about this in the much-read Underemployment post.
The pressure from academia (and downstream of that, prior authorization) to hypofractionate has created challenges, particularly because of the inequity / disparity between what a hospital receives vs what a freestanding center receives. The PPS-exemption furthers such disparities.
The CPT revisions will likely decrease the per patient reimbursement.
Consolidation leads to decreased competition and this creates downward pressure on income. If there is only one employer in town, it is difficult to negotiate. Many physicians have earned the same amount for years.
So… for the numerically inclined, I will introduce … The Parikh Equation
Key Takeaways:
Patient volume per RO will continue to decrease due to faster workforce growth relative to patient volume growth.
Fewer fractions per patient reduces income per patient, even if total patient numbers increase slightly.
Lower reimbursement per fraction further reduces total revenue.
Consolidation redistributes income, favoring larger centers over smaller, independent practices. Consolidation effects exacerbate the decline for independent or small-group ROs
Despite the offers people are getting out of residency, there is no way we can sustain our specialty’s current income level with the growth of physician supply and downward pressure on reimbursement. It’s simple math. Now, this is not to say anything will change soon. Most of us are employed and the hospitals may not notice the changes until a few years pass. Some practices will suddenly find a love for conventional fractionation or use more IMRT boosts for breast cancer or see more follow ups or find other ways to achieve their target income. Many centers have started treating benign conditions, as this is a growth area, but these are low revenue. Fortunately for patients, the number of cancer cases is essentially fixed and zero-sum, but this does not bode well for our specialty.
Obviously, if the 2026 CPT code revisions significant decrease reimbursement, then there is no turning back. If they substantially reduce the RVU values of what we do, it will be increasingly difficult to justify the status quo. We will have to accept lower incomes, and as frustrating as that is, it’s fine. We will have to accept lower incomes and as frustrating as that is, it is fine. This is a wonderful specialty and it’s a privilege to take care of these patients. But, we cannot sustain >$500-600k salaries for 6000-9000 RVUs - I don’t see how that works.
Now, ROCR.. If ROCR goes through in its current form at current rates proposed, then Medicare payments will be stabilized. i.e., $200 million in savings over 10 years is not going to hurt us—a drop in the bucket. But, this is for pure Medicare patients. Commercial insurers, Medicare Advantage and Medicaid will make changes based on the CPT revisions. I don’t see how they will continue to pay what they do today if the RVU values drop significantly for our bread and butter codes. I imagine that, overall, the specialty will see a decline in income of about 10-15% over the next 5 years or so. Some smaller centers will have to close, others will get swallowed up and more and more of us will be dependent on hospital employment. The younger generation of radoncs only know hospital employment, so I don’t think lack of ownership will bother them as much as it does many of us. They also did not live through the golden years, so they won’t feel the hit the way physicians in their 50s to 70s do.
The take home for this - the math is not in radiation oncology’s favor, but we have no idea what the future truly holds. The job itself remains as interesting and inspiring as it ever was. To the forum posters who are concerned… if you rotate and enjoy radiation oncology and it inspires you, do not worry - it is going to be okay - trust me! Despite what appears to be doom and gloom, almost all of my entire personal network of radiation oncologists loves their job and patients, feel well compensated and enjoy our niche of medicine. Don’t do it because of the money, but also don’t not do it because of the money. Decisions of this magnitude should be based on many factors - giving too much weight to income is risky. Specialties that no one wanted to do when I was in medical school are doing remarkably well, while other ones have floundered. We don’t know if a “new IMRT” will present and stabilize us in the future.
Personally, choosing radiation oncology has been a godsend. It’s allowed me to build a wonderful life, live in cool parts of the United States, build and maintain amazing relationships with patients and staff and earn a good income. I continue to nerd out on all things rad onc—reading journal articles, creating content for the podcast and here, and maintaining friendships with so many of you. Hell, my son’s middle name is the dose we treat with—yeah, I’m a super dork. I'm glad I found this field. Even with current concerns, if I was a medical student today, I’d still apply. If you like oncology, imaging and technology, this is the place to be.
Love you all,
Sim





Indeed, ROCR may offer some hope.. but analysis further shows it will just change our specialty's death from limb amputation to "hit by shotgun blast" as we bleed out perhaps slightly slower and less noticeably... all the while as PPSe slurps up more centers cheaply (distressed assets) and continues to happily charge away at 2-3x. The endgame is near...