Beyond B51 : Updating Our Playbook for Post-Mastectomy Radiation
Building Practical Algorithms for Breast RT Decisions
TL;DR - B51 was negative, here is how I treat these patients, scroll down to the flowcharts. For those that want to learn more ..
Breast cancer, the bread and butter of community radiation oncology, should not be very hard.
The decision points after surgery are:
Does this patient need radiation at all?
If yes, what are the volumes that need to be treated?
That’s all. Yes, dose plays a role, but 40-42.56 Gy / 15-16 Fx +/- 10 Gy / 4-5 Fx is a pretty good “one size fits all” approach. Some form of IMRT is used - either FiF/segments with forward planning, software like EZ Fluence that mimics inverse planning or “real” IMRT or VMAT with inverse planning. Certainly one can get into APBI and boluses and protons and such, but it all should be pretty simple.
So, say the answer to question 1 is yes, then what?
Breast or chest wall is always part of the target volume and should get RX dose. The coverage can be 95/95 or even 90/90 if necessary for OAR coverage and your outcomes will be good. Watch that V105!
Will you treat the regional nodes?
For the sake of discussion, let’s consider chest wall cases and PMRT. When I started residency, we treated anyone with 4 or more positive nodes. For patients with 1-3 positive nodes, we took into account patient age, size of tumor, grade, LVSI, margin status, # of nodes positive, # of nodes removed, ECE in nodes. We also could use nomograms to help us predict who may benefit from PMRT. However, some time later in my residency, the guidelines said to strongly consider PMRT to chest wall and regional nodes for patients with any positive nodes. So, most people tended to do that, rather than trying to estimate the potential benefit of a 63 yo woman with left sided IDC, +/+/-, grade 2, s/p MRM and chemotherapy, pT2N1M0 disease, 1/10 nodes positive, no ECE, no LVSI and negative margins. Most radoncs would just treat and I believe this to be defensible, though minimally beneficial for many patients.
If we decided to treat, our institutional training was to treat the chest wall, the supraclavicular region and level 3 of the axilla. If there were concerns about axillary recurrence, often times one could consider treating level 1 and 2, as well (if someone calls it a PAB, I’m gonna lose my mind). IMNs were almost never treated during my residency years, but that changed a few years later and some people always treated them, some people only treated if there was gross disease pre-treatment and other people based it on factors like location of tumor and number of nodes positive. I didn’t find any great resources that approached this systematically - it was truly choose your own adventure. If 5 radoncs saw this patient, there are at least 5 defensible ways to treat:
No PMRT at all
CW + SCV + level 3 axilla
CW + SCV + full axilla
Same as 2 + IMN
Same as 3 + IMN
For residents and new attendings, when you get out in the real world, if you do not have a system in place, it is daunting and decision paralysis can occur. I am here to tell you that you can make things very easy on yourself by working out a system for yourself that will take care of most cases that you see.
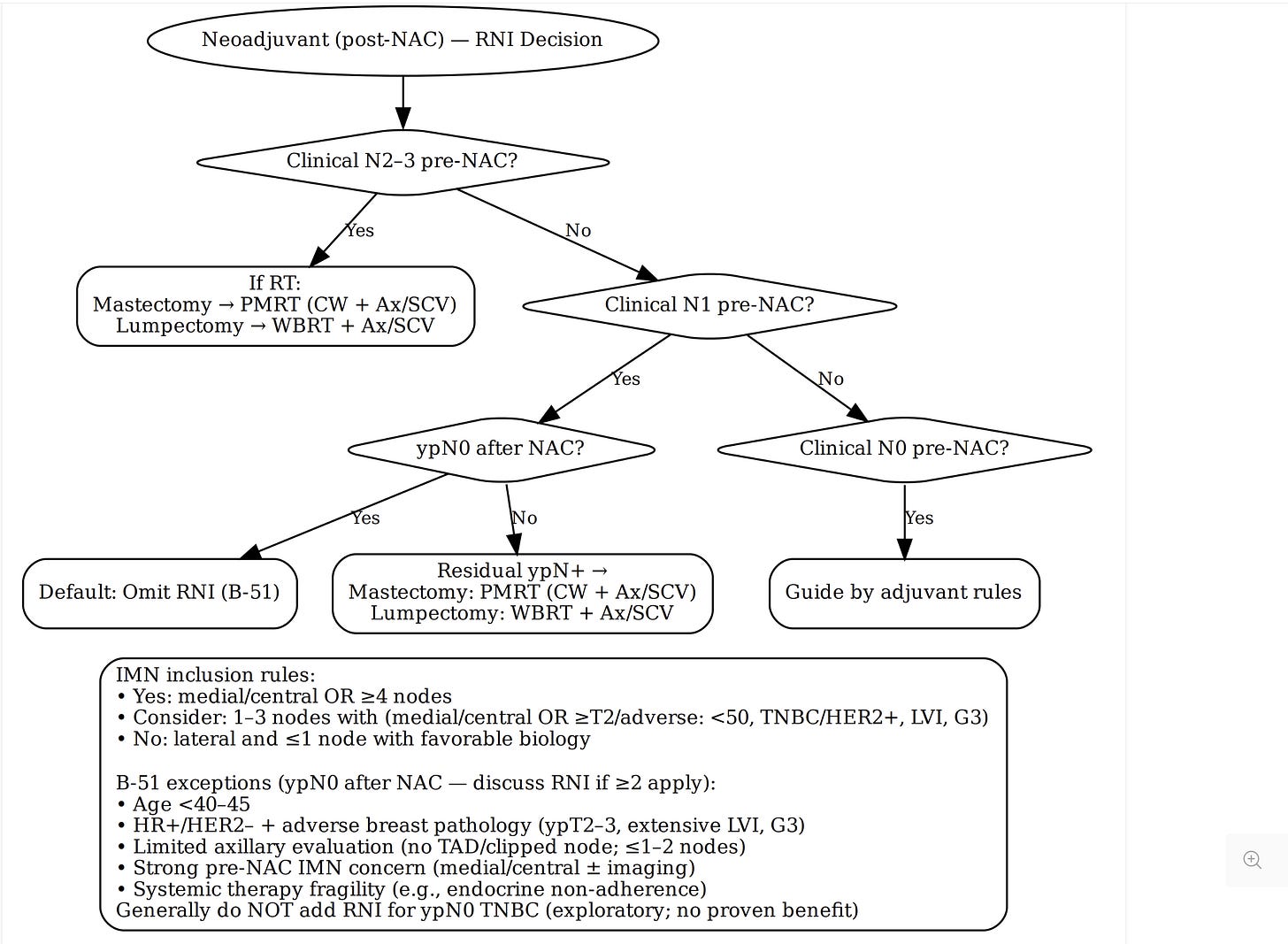
I had a system, but I needed to update it with the publication of NSABP - B51. This studied whether patients with positive nodes that were cleared after systemic therapy require RNI, or in the case of mastectomy, whether they need any RT at all. The patients treated with breast conservation all received whole RT to breast and they randomization was between RNI and no RNI. The patients with mastectomy were randomized to radiation to CW and RNI vs no RT at all. Everyone had comprehensive nodal radiation that included treatment of the IMNs.
I am not going to get into the details, as others have in detail, but it was a negative trial and there was no benefit for additional treatment. I had a dinner the other night in our breast working group and the medoncs and surgeons asked why radiation oncologists didn’t seem to believe in the study and routinely omit RNI or PMRT with RNI. Okay, I agree, my dinners seem much more boring than yours. Anyway, my brilliant partner (one of the authors of the study) explained the nuances of the study and I took notes. The main issue is that eligibility was broad, so many specific types of patients were underrepresented, so it is difficult to make blanket statements. I reviewed the publication. I reviewed the non randomized data. I reviewed the various interpretations of B51. I re-reviewed the Danish and British Columbia studies. I generated an algorithm and then had ChatGPT help me fine tune it. What came out is pretty good, if I do say so myself. For those starting out, this flowchart is systematic, allows for nuance and modifications based on specific factors, but it does not lock you into dogmatic treatment.
One part that may seem out of place is the consideration of chest wall RT only for certain intermediate risk patients in the adjuvant group. This has not been studied, but I kept it as an option for a few reasons. 1) 65-70% of locoregional recurrences are in the chest wall and the remainder are in the regional nodes 2) There is added toxicity by treating the regional lymph nodes 3) If you have an intermediate risk patient like the woman above, perhaps we say her overall risk is 12% (10-15% is a reasonable range). 8% of those are in the chest wall, 4 % in the nodes. By treating chest wall alone we reduce the risk to maybe 1-2% and then overall LRR is about 4-5%. If I have a hard time meeting OAR constraints, I have no worries about dropping coverage to something like 80% / 80%. And if you are doing that, one could make an argument just to leave them out. We know that it is defensible to not treat the patient to begin with, so this is a potential middle road. I wonder if anyone will ever study this approach. The only PMRT study I know that only treated the chest wall alone was a Chinese study looking at T1-T2N0M0 triple negative patients treated with adjuvant chemotherapy then randomized to chest wall RT vs no further treatment. PMRT to chest wall was associated with a >10% overall survival benefit, but this study appears mostly ignored.
First is the neoadjuvant chemotherapy patients, which considers the results of B51:
Next is the adjuvant chemotherapy patients.
I hope you find this helpful in generating your own way to treat these patients. Do not overthink it. Most answers are correct and more often than not, we confuse ourselves. For example, a patient comes to you that was eligible for both Z-11 and MA.20 which means whole breast RT alone works fine or it means treating the regional nodes will improve DFS. Who really knows? Believe one or the other and stick with it.
The risk of recurrence remains low. Be conservative in meeting OAR constraints and be comfortable with reducing coverage - i.e. APBI works so if you are only treating 90% of the breast PTV with 90% of the RX dose, as long as the tumor bed is covered by 95%, you are all good.
Breast often seems like the worst, but that’s because we overthink it. I’ve said to friends, if you’re a community generalist, you are a breast cancer specialist - you already know what to do. Develop a system, stick with it, adjust as new data comes out.
Love you all,
Simul



Thanks! Just curious- in your textual example of a low risk pT2N1 patient you state PMRT is likely minimally beneficial (I agree, see eg SUPREMO). Yet your flowchart algorithm treats these patients always? You’d just do CW alone if deescalating?
B-51 exceptions
HR+/HER2- + adverse breast pathology (ypT2-3, extensive LVI, G3)
Is there typo? HR+/HER2- maybe HR-/HER2+?